By Joellen Patterson, PhD, LMFT
The foundation of this small project was a curiosity about whether, and if so to what extent, Don Bloch’s (physician, key founder of the Collaborative Family Healthcare Association) ideals for integrated care as voiced at Wingspread (first CFHA meeting) have been realized in the world of integrated care today. C.J. Peek wrote an article nearly ten years ago about where integrated care stood in respect to Bloch’s ideals at that point in time, and this short paper is meant be a near 10-year follow-up to Peek’s work (Peek, 2015). This project was motivated by the ongoing selection process for a new Families, Systems, and Health (FSH) editor, in the hopes that a reflection of where integrated care was, where it stands now, and where it may would help inform the selection committee. (Since the inception of the project those editors have now been selected.)
From December 27, 2022 to January 27, 2023, the following people were interviewed about the state of integrated care, especially in comparison to its original formulation as presented at the 1994 Wingspread conference: Dr. C.J. Peek, Dr. Susan McDaniel, Larry Mauksch, Dr. John Rolland, Dr. Gene Kallenberg, Dr. Bill Doherty, and Dr. Mac Baird. These individuals were asked about successes of integrated care, current roadblocks to increased adoption and implementation of integrated care, the role of the family, and thoughts and ideas of future direction for FSH. Though many of the interviewees prefaced their answers by stating they had moved on from working in integrated care in the last ten or twenty years, nearly all still had insights about the successes and areas of growth for the field and for FSH.
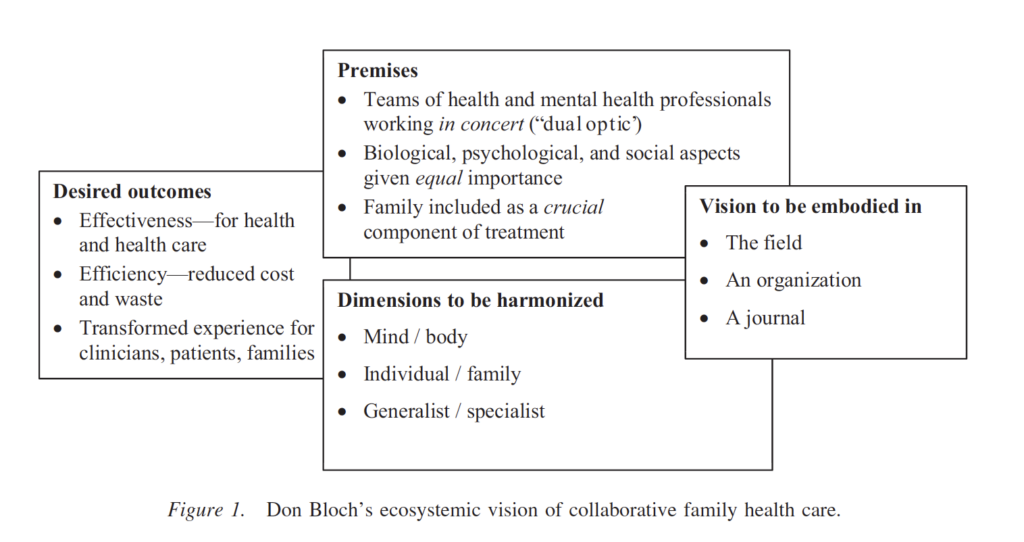
Don Bloch’s vision as visualized by C.J. Peek (Peek, 2015)
Interview Findings
All interviewees agreed that integrated care has made progress in the last 20-30 years. Some interviewees thought of this progress as more widespread acceptance of the importance of integrated care, while others pointed to the increased number of practices instituting (their own version of) integrated care. At the same time, interviewees were quick to point out roadblocks. One of the two primary roadblocks for increased adoption and implementation of integrated care is the lack of conducive financial payment systems. McDaniel sees the fee-for-service model as inhibiting further growth of integrated care and implementation of its central tenets. This was Peek’s opinion too, as he expressed that payment systems are still anchored in the mind-body split. At the same time, he notes that several sites have been able to take advantage of alternative payment schemes like shared savings and pay-for-performance, though these are still workarounds. The second primary roadblock expressed among interviewees is the “how to” of implementation, about which there still isn’t enough research. See below for more commentary on this.
Roadblocks for increased adoption and implementation of integrated care
- Existing payment models (e.g. fee-for-service) do not support high levels of integration
- Need more evidence (RCTs, or other studies with comparison groups) supporting effectiveness of integrated care
- Lack of unified conceptual definition of integrated care
- Mind-body division still prevails as dominant healthcare view
- Lack of manualized implementation strategies
- Lack of involvement of family
One of Bloch’s original visions for healthcare was that it would incorporate both the individual and the family. All interviewees agreed that the family is still not involved or utilized in integrated care. There were a variety of reasons posited for this idea. One was that there is no financial system (e.g. reimbursement) in place that rewards any involvement with the family. This problem is compounded by the public’s lack of awareness of why including the family might be beneficial, especially when many primary care appointments are preventative. Peek noted that one way in which family is involved is through healthcare systems’ involvement of communities, of which families are the primary unit of care.
Another part of Bloch’s vision was the balance between the mind and the body. While most interviewees still lamented healthcare’s stuck place in this split, there were some ideas about how insight into this faux-duality may be shifting. Peek mentioned that research about chronic illness, ACEs, health behavior changes, and depression as a “foreground” issue have all encouraged the medical field to see the mind and body as intermixed. Mauksch thinks, too, that that increased insight into the epidemiology of mental health issues have made integration more logical, as such epidemiology sees the mental and physical colliding. Despite these at least conceptual advancements into the shallow nature of the mind-body split, the dualism still dominates business models and inhibits further integrated care adoption.
A third part of Bloch’s vision was about the importance of striking a balance between generalists and specialists. Not many interviewees commented about this, but the ones who did agreed that there was there are still too much emphasis/reliance on specialists. At the same time, Rolland thought that it makes a lot of sense for families to be involved in specialty clinics because, presumably, the person is already sick.
In addition to being asked about Bloch’s original vision, interviewees were asked about CFHA, the role of research in supporting integrated care, and FSH. There was consensus among the interviewees about the unbalanced nature of CFHA’s member (physicians and behavioral health providers) makeup. There are various reasons for this. For one, as Mauksch put it, it’s never been that balanced. Another reason in Mauksch’s eyes is that physicians have less time and are faster moving than BHPs, and often don’t have the same research and academic training as do some BHPs. Third, many (if not most) physicians still don’t have the incentive to incorporate integrated care into their clinics because of their clinics’ clinical leadership and administration.
A number of interviewees had suggestions about research needed to advance integrated care. These suggestions fell mainly into two categories: proving the utility of integrated care and explaining the “how-to” implementation of integrated care. Many people advocated for the need for more studies with comparison groups illustrating the effectiveness of integrated care. Regarding the second point, many interviewees expressed the need for studies about how to “fit everything together” for an integrated care setting, including business model, delivery model, and education and training. In addition to these two main points, there were rumblings among several interviewees about how there isn’t even agreement in the research about what integrated care looks like (e.g. a singular model).
Some interviewees had thoughts about FSH and what types of articles it should publish. Rolland for example, thought the journal needs more conceptual papers (and fewer data-driven articles), needs to be more multi-disciplinary, and needs to refocus on how to make integrated care truly systemic. Mauksch had somewhat different ideas and expressed the negative consequences of contributors conflating the collaborative care approach and the PCBH approach, stating that PCBH does not have nearly the same strength of evidence as does the collaborative care approach. Kallenberg also had ideas for the journal and stated that there are too many special interest articles and one-off articles reviewing how integrated care was implemented at a single site. He suggested that the journal needs more papers about measuring the effects of integrated care, papers examining integrated care operational difficulties, and articles that target primary care physicians more in an attempt to realize the importance of integrated care. Thoughts and suggestions for FSH can be summarized by the following list:
Suggestions for FSH
- The journal needs fewer “one-off” studies about case successes
- The journal needs more rigorous studies involving comparison groups proving effectiveness of integrated care
- The journal needs more articles addressing workflow, training, and operational issues
- The journal needs to have articles that better attract physicians
- The journal needs more conceptual papers (Rolland)
Conclusion
In summary, while the field of integrated care continues to make advances, it still faces external impediments, like financial payment systems rooted in the mind-body split, as well as internal difficulties, like lack of a “one-size-fits-all,” or even a “one-size-fits-most” approach for implementation. Nevertheless, there is more support for the idea of integration and its potential benefits for patients, healthcare systems’ pocketbooks, and providers. It is an open question in what capacity FSH will propel integrated care going forward. Will it focus on disseminating rigorous research to further prove the efficacy of integrated care? Will it provide more manualized approaches for non-integrated healthcare systems to move toward integration? Will it be a platform for conceptual and experimental inquiry into how integrated care may look?
February, 2023
References
Peek, C. J. (2015). Don Bloch’s vision for collaborative family health care: progress and next steps. Families, Systems & Health, 33(2), 86.
JoEllen Patterson, PhD, LMFT, is Professor in the Marital and Family Therapy Program at the University of San Diego. She is also Associate Clinical Professor of Family Medicine, Global Health, and Psychiatry at the University of California, San Diego, School of Medicine.
__________________________________________________________________–